Otitis Externa
What is otitis externa?
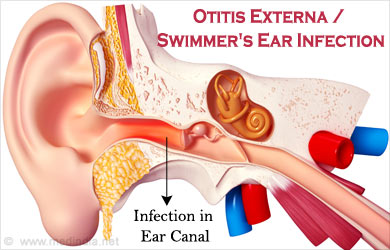
Inflammation of any part of the outer ear. The ear can be divided into three sections: the outer ear, middle ear and inner ear. The outer ear can be further divided into the auricle (the external part of the ear that is visible to the naked eye) and the auditory canal (also known as the external auditory meatus/ear canal). Any inflammation within the outer ear is termed otitis externa.
What are the symptoms?
The symptoms will vary according to the type of otitis externa and the severity.
Symptoms may include:
- Earache (otalgia)
- Tinnitus
- Hearing loss
- Itchy ear
- A sensation of fullness in the ear
- Signs include: redness (erythema), swelling (oedema)
- Pain
- Fever
- Otorrhea (clear or pus discharge from the outer ear)
- Inflammation may spread to the face or neck (rarely occurs)
- Signs and symptoms may occur in one ear or in both ears (rarely occurs in both ears)
Who does the condition affect?

It can affect individuals of any age. Some people are more prone to contracting an outer ear infection. For example, people who swim, dive or participate in water based activities are more likely to develop the condition. Due to the higher incidence of contraction for swimmers’, otitis externa is sometimes known as swimmer’s ear. Humid weather also increases the likelihood of developing an outer ear infection. The use of earplugs, hearing aids, cotton buds and any form of outer ear trauma can irritate the auditory canal and are risk factors for developing outer ear infections. Additional risk factors include a history of eczema, asthma, hay fever, diabetes mellitus (type 1 diabetes), malnutrition, AIDS and leucopenia.
Who does the condition affect?
It can affect individuals of any age. Some people are more prone to contracting an outer ear infection. For example, people who swim, dive or participate in water based activities are more likely to develop the condition. Due to the higher incidence of contraction for swimmers’, otitis externa is sometimes known as swimmer’s ear. Humid weather also increases the likelihood of developing an outer ear infection. The use of earplugs, hearing aids, cotton buds and any form of outer ear trauma can irritate the auditory canal and are risk factors for developing outer ear infections. Additional risk factors include a history of eczema, asthma, hay fever, diabetes mellitus (type 1 diabetes), malnutrition, AIDS and leucopenia.
How long does it last for?
Generally the condition will resolve within 2-3 days following medical treatment. Sometimes it does not resolve within this time frame and further medical examination is necessary. Without treatment otitis externa may progress into a more severe form, like necrotising otitis externa, which can be fatal.
What causes the condition?
A bacterial skin infection of the outer ear is the most common cause of otitis externa. It can also be caused by a fungal or viral infection.
A number of changes within the outer ear make it easier for these microorganisms to grow resulting in an outer ear infection. A reduction of ear wax (cerumen) in the outer ear allows bacteria to grow in the auditory canal because the acidity of ear wax prevents bacterial growth. Reduced ear wax can be caused by frequent swimming or water based activities. Excessive ear wax in the auditory canal may trap microorganisms and lead to infection. Trauma to the outer ear may breach the skin and cause an infection. The infection triggers the inflammation, redness and other signs and symptoms of otitis externa.
How does otitis externa cause hearing loss?
The infection in the outer ear may result in a blockage of the outer ear. This blockage may be due to inflammation, pus/liquid build up or a narrowing of the auditory canal. Any blockage within the ear may prevent the transmission of sound resulting in a hearing loss. This type of hearing loss is termed a conductive hearing loss (for more information on conductive hearing loss click here) because the hearing loss is caused by a problem within the outer ear.
How long does the hearing loss last for?
The hearing loss is generally temporary and will resolve as soon as the infection resolves.
What are the different types of otitis externa (OE)?
| Type of Otitis Externa | Description |
|---|---|
| Acute diffuse OE | -Most common type of OE -Signs and symptoms may include: itchiness, otalgia (earache), hearing loss , inflammation of the auditory canal, jaw pain, redness, swelling and outer ear discharge -Frequently occurs in swimmers -Rapid onset |
| Acute localized OE (also known as furunculosis) | -Infection of a hair follicle within the outer ear -Signs and symptoms localised to the region of the infected hair follicle |
| Chronic OE | -Same signs and symptoms as acute diffuse OE, however it lasts for longer and carries the risk of additional complications -Lasts for over 6 weeks |
| Necrotizing OE | -A malignant infection -Spreads to internal tissues near the outer ear -Severe earache -More likely to affect those with a compromised immune system (individuals taking medications that suppress the immune system) -Individuals with necrotizing OE should be referred to an ENT surgeon |
| Otomycosis OE | -Caused by a fungal infection |
How is the condition examined?
If you think you have OE you should visit your doctor. An audiologist will conduct a hearing assessment and refer you to a doctor if you have OE so that the correct medication can prescribed.

The clinician will gather a case history by asking you about your medical history and asking you questions about your presenting problems. An otoscope will be used to examine your ear. An otoscope is an instrument that allows for the visualisation of the eardrum and the auditory canal. If you have OE this otoscopic examination will reveal some or all of the following signs: redness, outer ear discharges (liquid or pus in the outer ear), inflammation, swelling, a narrowed auditory canal and an inflamed eardrum.
An audiologist will conduct a hearing test to determine whether there is a hearing loss and to determine the severity of the hearing loss. A doctor may take a culture sample for laboratory testing (to determine the type of infection, e.g. bacterial, fungal or viral), refer you for medical imaging or make a referral to an ENT surgeon. Culture sampling, medical imaging and referrals to an ENT surgeon usually are not required.
How is OE treated?
There are a number of treatment options available for OE. The most appropriate treatment will depend on the type of OE, the cause, the severity and your individual circumstances. The main treatment options include medication to treat the infection, pain management through medication, avoiding a lifestyle that fosters ear infections and surgical treatment for more extreme cases. Hearing aids are usually not required since the hearing loss will resolve when the infection clears (and hearing aids will irritate the inflamed outer ear). However, bone conduction hearing aids may be appropriate in cases of chronic/necrotising OE (for more information on hearing aids click here).
Medications
- Antibiotics for OE caused by bacterial infections
- Painkillers to manage earaches
- Antifungal medications for OE caused by fungal infections
- Antiviral medications for OE caused by viruses
Lifestyle changes
Certain environments and behaviours can increase the likelihood of developing OE. Avoiding swimming and humid environments can help prevent a recurrence of OE. Reducing how regularly you clean your ears with cotton buds can also help prevent a recurrence as this can aggravate the outer ear and make it easier for microorganisms to grow.
Surgical intervention
Surgical intervention is only required in the more severe cases of OE. Surgery may involve the removal of damaged tissue, the removal of an abscess (pus filled area of skin) or draining swollen tissue.